Abstract
Introduction: Prior studies have demonstrated that racial/ethnic minority groups and patients with low socioeconomic status (SES) have worse overall survival (OS) after allogeneic hematopoietic stem cell transplant (allo-HCT). Whether the racial and SES disparity in outcomes persists and possibly may even be exacerbated in allo-HCT recipients with chronic graft-versus-host disease (cGVHD) is unknown. Certain aspects of cGVHD such as the need for long term care, prolonged immunosuppressive treatment, and close follow up for complications may exacerbate racial and SES disparities. In the current study, we analyzed the association of race/ethnicity and SES with the incidence of cGVHD and compared the long-term outcomes of allo-HCT survivors with cGVHD by race/ethnicity and SES.
Methods: The study population comprised 14,825 adults with acute myeloid leukemia (AML), acute lymphocytic leukemia (ALL), myelodysplastic syndrome (MDS), or myeloproliferative neoplasm (MPN) who received first allo-HCT between 2008-2018 in the United States. Residential ZIP code at the time of allo-HCT was used to estimate annual household income as the measure of SES. Patients with relapse of the primary disease prior to diagnosis of cGVHD were excluded. The incidence of cGVHD was calculated using the cumulative incidence estimator. Cox regression models were used to determine whether race/ethnicity and SES were associated with overall survival (OS), treatment related mortality (TRM) and relapse among patients with cGVHD. A stepwise backward variable selection was used to develop models for each outcome with a threshold of 0.05 for retention in the model. The main variable was then forced into the models. Interactions between the main variable and the adjusted covariates were tested at the significance level of 0.01.
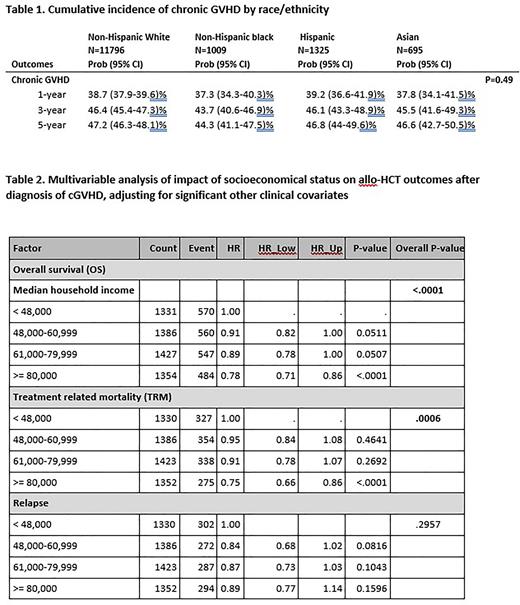
Results: Patients were reported to be Non-Hispanic White (W) (n=11,796), Non-Hispanic Black (B) (n=1,009), Hispanic (H) (n=1,325), and Asian (A) (n=695). A total of 5,600 relapse-free allo-HCT recipients developed cGVHD. There was no significant difference in cumulative incidence of cGVHD based on race/ethnicity (p=0.49, Table 1) or SES (p=0.44). In the multivariable analysis, we observed no significant differences in OS (p=0.15), TRM (p=0.11) and relapse (p=0.03) in patients with cGVHD based on race and ethnicity adjusted for patient-, disease- and transplant-related covariates.
SES (household income, with or without adjustment for health insurance status) was significantly associated with OS (p<0.0001) and TRM (p=0.0006). More specifically, the highest quartile of household income (≥ $80,000) was associated with improved OS (HR 0.78, CI 0.71-0.86, p< 0.0001) and reduced TRM (HR 0.75, CI 0.66-0.86, p< 0.0001) compared with the lowest household income quartile (< $48,000) (Table 2). There was no association between the SES and relapse among patients with cGVHD (p=0.29).
Conclusions: Our study highlights that low SES, regardless of race/ethnicity, has a negative impact on outcomes after diagnosis of cGVHD. Disparities in outcomes solely based on race/ethnicity were not evident among patients with cGVHD. Future studies are needed to determine if people with low SES and cGVHD have disproportionately worse outcomes than those with low SES without cGVHD. If they do, then optimizing the health care resources available to cGVHD patients with low SES may improve long-term outcomes.
Disclosures
Pidala:BMS: Research Funding; Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees; Incyte: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Research Funding; Takeda: Research Funding; CTI Biopharma: Consultancy, Membership on an entity's Board of Directors or advisory committees; Syndax: Consultancy, Membership on an entity's Board of Directors or advisory committees; Regeneron: Consultancy, Membership on an entity's Board of Directors or advisory committees; Johnson and Johnson: Research Funding; Pharmacyclcis: Research Funding; Abbvie: Research Funding. Kitko:Horizon Therapeutics: Consultancy. Lee:Mallinckrodt, Equillium: Consultancy; Amgen, AstraZeneca, Incyte, Kadmon, Novartis, Pfizer, Syndax, Takeda: Research Funding; Janssen: Other: Provision of study medication; National Marrow Donor Program: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal